Strabismus, commonly referred to as crossed eyes or squint, is a condition characterized by the misalignment of the eyes. In individuals with strabismus, one eye may turn inwards, outwards, upwards, or downwards while the other eye remains straight. This misalignment can be constant or intermittent and may result in various visual disturbances, including double vision (diplopia), reduced depth perception, and amblyopia (lazy eye).
Strabismus can manifest in different forms, including:
Treatment for Strabismus:
Treatment for strabismus aims to improve eye alignment, restore binocular vision, and prevent vision loss.

Nystagmus is a condition characterized by involuntary, rhythmic movements of the eyes, which may occur horizontally, vertically, or in a rotary fashion. These eye movements can be rapid and jerky, slow and oscillatory, or a combination of both. Nystagmus can affect one or both eyes and may result in various visual disturbances, including reduced visual acuity, blurred vision, and oscillopsia (illusion of motion).
Causes of Nystagmus:
Nystagmus can be associated with various factors, including:
Treatment for Nystagmus:
Treatment for nystagmus depends on the underlying cause, severity of symptoms, and impact on visual function.

Lazy eye, medically known as amblyopia, is a vision development disorder that typically begins in childhood. It occurs when one eye has significantly better visual acuity than the other, often due to abnormal visual input during the critical period of visual development. This condition can lead to reduced vision in the affected eye if not detected and treated early.
Amblyopia can be caused by various factors, including:
Strabismus: Misalignment of the eyes, where one eye turns inwards, outwards, upwards, or downwards, can lead to amblyopia in the misaligned eye.
Refractive Errors: Significant differences in refractive error (such as nearsightedness, farsightedness, or astigmatism) between the eyes can cause amblyopia in the eye with the more significant refractive error.
Visual Deprivation: Conditions that obstruct or limit vision in one eye during early childhood, such as congenital cataracts, ptosis (drooping eyelid), or significant uncorrected refractive errors, can result in amblyopia.
Treatment of Amblyopia:
The goal of amblyopia treatment is to improve vision in the affected eye and promote binocular vision.

Blocked tear duct, medically known as dacryostenosis, is a common condition in infants and occasionally occurs in adults. It occurs when the tear duct (nasolacrimal duct), which normally drains tears from the eyes into the nose, becomes partially or completely obstructed. This obstruction can lead to excessive tearing, discharge from the eyes, and discomfort.
The primary symptom of blocked tear ducts is excessive tearing, which may be accompanied by:
In infants, blocked tear ducts may also lead to recurrent eye infections (conjunctivitis) or a bulging area near the inner corner of the eye (dacryocystocele) due to accumulation of fluid.
Treatment of Blocked Tear Duct:
Treatment for blocked tear ducts depends on the underlying cause, severity of symptoms, and age of the patient.

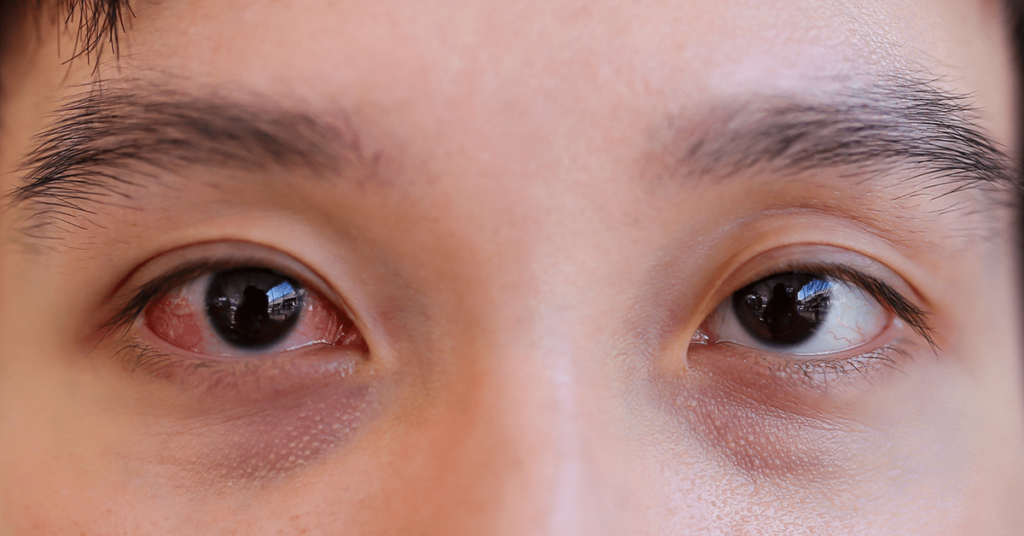
Conjunctivitis, commonly known as pink eye, is an inflammation of the conjunctiva—the thin, transparent membrane that covers the white part of the eye and lines the inner surface of the eyelids. Allergic and viral conjunctivitis are two common types of conjunctivitis, each with distinct causes, symptoms, and treatments.
Treatment of Viral Conjunctivitis:
Viral conjunctivitis is typically self-limiting and resolves on its own within one to two weeks. Treatment focuses on relieving symptoms and preventing transmission to others. Treatment options may include:
Cold Compresses: Applying cold compresses to the eyes can help alleviate discomfort and reduce inflammation.
Artificial Tears: Over-the-counter artificial tear drops or lubricating eye gels can help soothe dryness and irritation.
Antiviral Eye Drops: In severe cases caused by herpes simplex virus (HSV), antiviral eye drops or ointments may be prescribed to shorten the duration of symptoms.
Hygiene Measures: Practice good hygiene, such as frequent handwashing, avoiding touching or rubbing the eyes, and disinfecting surfaces to prevent the spread of the virus.
A corneal abrasion refers to a scratch or injury on the surface of the cornea—the clear, dome-shaped outermost layer of the eye responsible for focusing light. Corneal abrasions can result from various causes, including foreign objects, contact lenses, trauma, or underlying eye conditions.
Common causes of corneal abrasions include:
Foreign Objects: Dust, sand, metal particles, or other foreign objects can scratch the surface of the cornea if they come into contact with the eye.
Contact Lenses: Improper insertion, removal, or cleaning of contact lenses can cause scratches on the corneal surface.
Trauma: Accidental eye injuries, such as getting poked in the eye with a finger or blunt object, can result in corneal abrasions.
Underlying Eye Conditions: Dry eye syndrome, corneal dystrophies, or recurrent corneal erosion syndrome can increase the risk of corneal abrasions.
Treatment of Corneal Abrasion:
Treatment for corneal abrasions aims to relieve symptoms, promote healing, and prevent complications.

A stye, also known as a hordeolum, is a common eyelid infection or inflammation that typically occurs at the base of the eyelashes or within an oil gland of the eyelid. It appears as a painful, red bump resembling a pimple or boil and can occur on the inside or outside of the eyelid. If a stye persists and becomes a painless, non-infectious lump, it is then referred to as a chalazion.
Styes are usually caused by bacterial infection, most commonly Staphylococcus aureus bacteria. Other factors contributing to styes include:
Treatment of Stye:
Most styes can be treated at home and typically resolve on their own within a week or two.

Myopia, commonly known as nearsightedness, is a refractive error of the eye that affects a person’s ability to see distant objects clearly while near objects appear in focus. It occurs when the eyeball is too long or the cornea is too steeply curved, causing light rays to focus in front of the retina instead of directly on it. This results in blurred distance vision, while close-up objects can still be seen clearly.
The exact cause of myopia is not fully understood, but it is believed to involve a combination of genetic, environmental, and lifestyle factors, including:
Genetics: Myopia tends to run in families, suggesting a strong genetic component. Children with one or both parents who are nearsighted are more likely to develop myopia themselves.
Eye Growth and Development: Myopia often develops during childhood and adolescence as the eyeball continues to grow and elongate. Excessive elongation of the eyeball can lead to increased nearsightedness.
Environmental Factors: Prolonged near work activities, such as reading, using computers, or focusing on digital screens for extended periods, may contribute to the development and progression of myopia, particularly in children.
Outdoor Exposure: Studies suggest that spending time outdoors, especially during childhood, may help reduce the risk of myopia development and progression.

Refractive errors are common vision disorders that occur when the shape of the eye or the curvature of the cornea (the clear front surface of the eye) prevents light from focusing correctly on the retina, resulting in blurred or distorted vision. Refractive errors can affect people of all ages and can be corrected with eyeglasses, contact lenses, or refractive surgery.
The exact cause of refractive errors is not always known, but several factors may contribute, including:

Mon 07:30 am – 05:00 pm
Tue 07:30 am – 05:00 pm
Wed 07:30 am – 05:00 pm
Thu 07:30 am – 05:00 pm
Fri 07:30 am – 05:00 pm
Sat By appointment
Sun Closed
Copyright © 2024, Stewart Eye Co, All Rights Reserved. Designed By Aj codegenius